Pancreas Cancer Surgery (Head) | Whipple Procedure
Pancreas is a vital retroperitoneal organ which secretes juices that help in digestion of fats & proteins and various hormones such as insulin that regulates blood sugar levels. Pancreas is anatomically divided into three parts: head, body and tail. Treatment of pancreas cancer depends on the location of the tumor – surgery for cancer of head & neck is Whipple’s procedure (pancreatoduodenectomy) whereas cancer of body & tail is treated by distal pancreatectomy.
Cancer of Head of Pancreas & Periampullary region
A carcinoma arising within 2 cm of the ampulla of Vater (i.e. the head of pancreas, ampulla, distal common bile duct and descending duodenum) are collectively referred to as ‘periampullary carcinoma’.
Even though the presentation, investigations and surgical treatment of the periampullary carcinoma is similar, location of the primary tumor is one of the important prognostic factors for perioperative and long term outcome.
The common symptoms at the time presentation for these cancers include: Weight loss, jaundice, pain abdomen, anorexia, dark urine, pale stools or generalized itching.
What is the preoperative work up for cancer head of pancreas & periampullary region?
These cancers are aggressive tumors which usually present at an advanced stage. Moreover these tumors occur predominantly in the elderly population who often have significant co-morbidities. Consequently only 15 – 20% of all patients are fit for pancreatoduodenectomy; others are suitable only for palliative therapy.
Thus, the objectives of managing a patient with suspected cancer involving this region are:
1. Establish the diagnosis
2. Assess fitness for major surgery
3. Meticulous preoperative staging so that only the patients with a curative intent should undergo exploration. A triple phase contrast enhanced CT scan of the whole abdomen (pancreas protocol) is the preferred imaging investigation. Contrast enhanced MRI with MRCP may also be used for staging purposes. In patients with resectable tumors CT scan of chest with or without contrast is done to exclude spread of cancer deposits in lungs. Endoscopic ultrasound may be performed for fine needle aspiration cytology (FNAC), when the tumor has doubtful resectability, plan for neoadjuvant therapy or for characterization of rare tumors.
The current available evidence does not support a routine ERCP intended to decrease preoperative bilirubin levels. An ERCP is required only in selected patients – with cholangitis, when an early surgery is not feasible due to logistic or medical problems or when the patient is planned for neoadjuvant therapy.
Whenever ERCP is being planned, it should always be performed after CT scan of the abdomen.
In cases of Ampullary & duodenal cancers biopsy confirmation is usually straight forward. For cancer involving head of pancreas & distal bile duct in the appropriate clinical setting a histological confirmation although desirable is not mandatory. If there is doubt in diagnosis or neoadjuvant therapy is required then EUS guided FNAC is the preferred technique for this purpose.
The tumor marker for these cancers is CA 19-9. This has no role for confirmation of diagnosis. However baseline values have a role in subsequent follow up.
a. Curative surgery
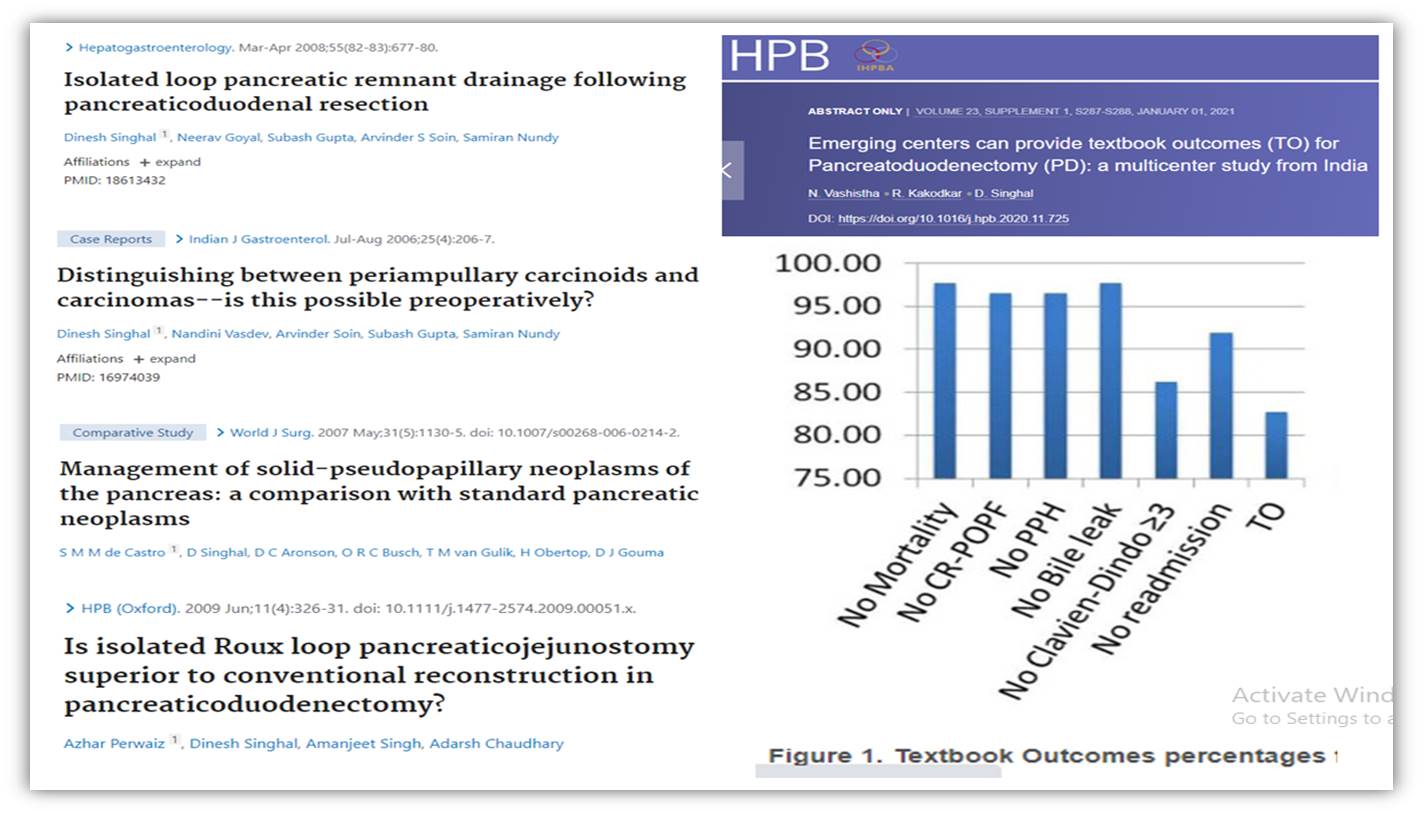
Whipple’s procedure (Pancreatoduodenectomy) remains the only available curative treatment for cancer of head of pancreas & periampullary region. At specialized centers, the procedure can now be accomplished with a mortality ranging between 1-5% and morbidity rates up to 40%.
The commonest complication following surgery is delayed gastric emptying while leak from pancreatico-enteric anastomosis is the most dangerous complication.
The Whipple procedure, also known as a pancreaticoduodenectomy, is a surgical procedure used to treat pancreatic cancer. This complex operation involves the removal of the head of the pancreas, the duodenum, a portion of the stomach, the gallbladder, and the bile duct.
The Whipple procedure for Pancreatic Cancer Head Surgery is typically performed on patients with tumors that are confined to the head of the pancreas and have not spread to other organs or tissues. The whipple procedure is not recommended for patients with more advanced cancers or those who are not healthy enough to undergo a major surgical procedure.
During the Whipple procedure, the surgeon makes an incision in the abdomen and carefully removes the affected organs and tissues. The remaining portions of the pancreas, stomach, and bile duct are then reconnected to allow for the normal flow of digestive enzymes and bile.
b. Palliative management
Endoscopic stenting (biliary / antral) or surgical double bypass (which can now be accomplished with low complications) are acceptable palliative procedures. The choice depends on available local expertise.
Pancreatic cancer is diagnosed as BRPC or LAPC if involvement of surrounding vascular structures precludes primary (upfront) resection. Approximately 30% of pancreatic cancer patients are identified as BRPC or LAPC. With combined modality treatment downstaging of the tumor is possible in many patients and Whipple’s procedure is possible with good long term outcomes (R0 resection).
The patients who do undergo curative surgery with surgical margins free of tumor have a median survival of 12 – 20 months; a margin positive resection confers no survival advantage and has an outcome similar to that of local unresectable disease.
The 5 year survival ranges between 15% (head of pancreas) to 60 % (duodenum).
Patients in whom the disease has spread to lymph nodes on final histopathological examination of surgical specimen are likely to benefit from chemotherapy.